
Possibly the most misunderstood surgical technique in spinal diseases treatment. It has been applied to almost all spinal diseases, from the cervical to the lumbar spine and maybe to an exaggerating degree. However, this is usually the only indicated and effective treatment method.
Definition
What does this term mean?
Spinal fusion is every surgical method that aims at stabilizing the spinal vertebrae and the disc among the vertebrae, with the assistance of metal materials and bone implant and its goal is the achievement of natural bone connection of the involved vertebrae.
When is spinal fusion indicated?
This depends on the possibility of causing spinal instability because of the disease or because of the attempted surgical treatment, which is usually performed through the removal of a bone part (joint, etc.) of the spine. In the case of iatrogenic instability, the spinal fusion indication is relevant as it’s not always a given and it is often defined at the time of the operation according to the size of the bone removal. There are, however, cases where spinal fusion is definitely indicated since the disease has already (during the treatment period) caused spinal instability, for example vertebrae fractures (60–100% of the vertebral anteroposterior diameter or the equivalent damage of a vertebra by a tumor). In these cases, when these are accompanied by bone marrow or nerve damages, spinal fusion application is extremely urgent in order to speed up the decompression of the most sensitive nervous tissue—which if it dies, it can’t be reborn, and this results in the permanence of severe neurological symptoms.
Consequently, spinal fusion is not only safe but also the only effective treatment that can save patients’ mobility. Patients who could otherwise become permanently disabled, stuck in wheelchairs, and would suffer severe neurological disorders related to urination, defecation, and erection.
What are the main spinal fusion techniques?
There are many spinal fusion surgical techniques and the selection of the right technique depends on the position of the damage that needs to be treated. Therefore, the techniques are classified as anterior, posterior, and lateral techniques, according to the damage approach.
We also distinguish them in classic and minimally invasive techniques, according to the size of the muscle ablation of the muscles surrounding the spine.
No matter the technique performed, general anesthesia is required and the precision and the safety of the spinal fusion is increased by the assistance of additional modern techniques, such as neuronavigation and the neuromonitoring
Please read below for the most important spinal fusion methods according to the position on the spine where they will be performed, and also for the most important advantages and disadvantages of the modern techniques compared with the classic ones.
Anterior cervical spinal fusion
It concerns cervical spine cases that are located in front of the bone marrow.
The damage is approached through a small horizontal incision 4–5cm long in the right anterior cervical area. The incision—if possible—is on a natural skin fold in order to make the postoperative scar almost invisible.
With the assistance of the portable X-ray machine (C-arm), the vertebra or the intervertebral disc that needs to be removed is located. Then, either the microdiscectomy is performed (removal of the suffering intervertebral disc) or the somatectomy (removal of a part of the vertebra) with the assistance of a microscope in order to prevent any iatrogenic damage of the bone marrow or the cervical nerve roots. The space that is created is usually filled in with implants (PEEK cage or titanium cage) and bone implant (either human or animal). In certain special cases, spinal fusion may be completed with the insertion of a thin metal plate, which is placed in the anterior surface of the spine with screws.
Anterior cervical approach, cervical discectomy, and spinal fusion with the use of self-locking PEEK cages and bone implant (ACDF A4-A5, A5-A6). [image taken from my personal archive]
Posterior cervical spinal fusion
It concerns cases of the cervical spine that are located behind the bone marrow, such as the yellow ligament thickening and cervical stenosis. In these cases, sometimes extended cervical laminectomy (for bone marrow decompression) is required and it can be combined with posterior spinal fusion with screw placement in the lower cervical spine (Magerl, Roy-Camil, Hand technique, etc.)
in order to prevent the postoperative instability of the area or the iatrogenic kyphosis of the cervical spine.
General anesthesia is administered and the patient lies face-down. A vertical incision in the middle of the neck is done and neck muscle ablation is performed. A surgical microscope is not usually required in this operation. The screw placement is done with the assistance of the X-ray machine (C-arm). The patient uses a semi-hard cervical collar for 6–8 weeks postoperatively.
Posterior lumbar fusion (lumbar, thoracic, or lumbar-thoracic)
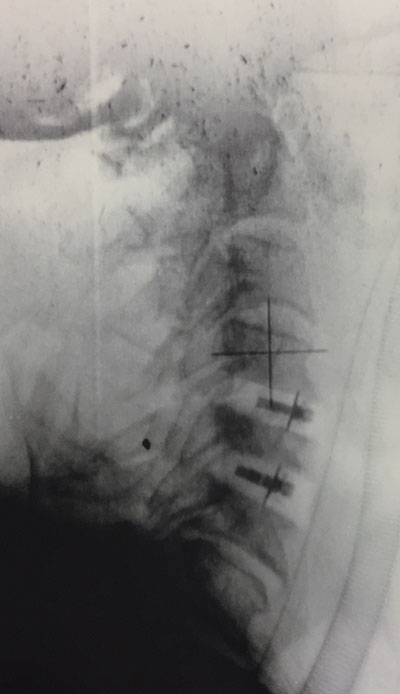
This is the most common spinal fusion technique in the lumbar spine. Instable fractures in the lumbar and lumbar-thoracic area are the best indication for this technique.
It is performed under general anesthesia and the patient face-down, since the goal is to approach the spine from behind (posterior access). The incision is done in the middle, right above the spine and its length depends on the number of vertebrae that will be screwed. Two screws are placed in each vertebra, one on the right and one on the left, with the assistance of X-ray guidance (C-arm) or neuronavigation.
Following the screw placement, wide decompressive laminectomy is performed. It is wide because the spinal stabilization has been ensured with the placement of two bars and transverse bridges between them. Finally, the bone implants are placed. These implants will help in the development of new bone, which will permanently connect the vertebrae (bone spinal fusion) that have been tied with metal materials (titanium or stainless steel) for spinal fusion.
A 3- or 4-day hospitalization is required for this method. Between the 8th and the 10th postoperative day, the clip or sutures removal is required.
The patient can start moving the next postoperative day, once the drain tube that is placed at the end of the operation is removed. The use of a lumbar brace is required.
The loss of blood during the operation depends on the extension of the operation but it is replaced with blood transfusion. Therefore, blood donation by 2 or 3 people is required preoperatively.
The loss of blood is decreased both intra- and postoperatively by an 8-day discontinuation of antiplatelet drugs (Salospir, Ticlid, Plavix, Iscover, etc.) and their replacement by heparin injections of low molecular weight (Clexane, Fraxiparine, Ivor, etc.).
Posterior lumbar interbody fusion (PLIF)(PLIF)
As with the aforementioned method, general anesthesia is required and the patient lies face-down. Usually, the required incision is smaller compared to the one in the posterior lumbar fusion because the discectomy incision is usually enough. Before the performance of this technique, bilateral discectomy is always performed with the assistance of a microscope. The space that is created between the two lumbar vertebrae is filled in with two implants either by titanium (Β-Τwins) or by PEEK (Polyether ether ketone: biocompatible polymer) and bone implant, usually in a paste format in order to keep the distance between the two vertebrae as well as to promote the completion of the bone connection (fusion).
As with the lumbar fusion, a 3- or 4-day hospitalization is required for this method. Between the 8th and the 10th postoperative day, the clip or sutures removal is required.
The patient can start moving the next postoperative day, once the drain tube that is placed at the end of the operation is removed. The use of a lumbar brace is required.
The loss of blood during the operation depends on the extension of the operation but it is replaced with blood transfusion. Therefore, blood donation by 2 or 3 people is required preoperatively.
The loss of blood is decreased both intra- and postoperatively by an 8-day discontinuation of antiplatelet drugs (Salospir, Ticlid, Plavix, Iscover, etc.) and their replacement by heparin injections of low molecular weight (Clexane, Fraxiparine, Ivor, etc.).
Posterior transforaminal lumbar interbody fusion (TLIF)(TLIF)
The posterior transforaminal lumbar interbody fusion (TLIF) is similar to the aforementioned technique (PLIF) and is the most advanced since it only requires unilateral discectomy and complete removal of the facet in order to create the required space for the placement of a banana-shaped implant by PEEK between the two vertebrae.
The posterior transforaminal lumbar interbody fusion (TLIF) is similar to the aforementioned technique (PLIF) and is the most advanced since it only requires unilateral discectomy and complete removal of the facet in order to create the required space for the placement of a banana-shaped implant by PEEK between the two vertebrae.
As with the lumbar fusion, a 3- or 4-day hospitalization is required. Between the 8th and the 10th postoperative day, the clip or sutures removal is required.
The patient can start moving the next postoperative day, once the drain tube that is placed at the end of the operation is removed. The use of a lumbar brace is required.
The loss of blood during the operation depends on the extension of the operation but it is replaced with blood transfusion. Therefore, blood donation by 2 or 3 people is required preoperatively.
The loss of blood is decreased both intra- and postoperatively by an 8-day discontinuation of antiplatelet drugs (Salospir, Ticlid, Plavix, Iscover, etc.) and their replacement by heparin injections of low molecular weight (Clexane, Fraxiparine, Ivor, etc.).
360° lumbar spinal fusion
The combination of the posterior lumbar fusion with the posterior lumbar interbody fusion (PLIF) or the posterior transforaminal lumbar interbody fusion (TLIF) leads to the 360-degree lumbar spinal fusion, that is the placement of spinal fusion materials all around the involved vertebrae, from behind toward the front. This technique is usually required in cases where the bone connection hasn’t been achieved through a single spinal fusion technique (cases of pseudojoint creation) or cases where the difficulty in the bone connection achievement is expected (cases of severe osteoporosis).
This is the most modern spinal fusion technique. It is basically the posterior lumbar spinal fusion with the use of screws and bars that are placed percutaneously (without a long incision but with several small incisions of 2cm long each) with the assistance of a portable X-ray machine (C-arm).
It is classified as a minimally invasive spinal surgery, just like kyphoplasty and vertebroplasty, because the interference with the healthy tissues surrounding the vertebrae is very small. For this reason, the loss of blood is minimal and blood transfusion is almost never required. Postoperative pain is also minimal, if any, and this allows for a swift recovery and the patient’s return to everyday activities. The disadvantage of this method is that several incisions are required.
The definite indication for this method is the spinal instability (spondylolisthesis or vertebra translocation and instable fractures) to one or two levels, with or without stenosis or disc herniation. Performing this technique, two things are achieved: the indirect decompression of the nerve elements with the spondylolisthesis reduction, and the direct decompression (laminectomy, discectomy) using the existing incisions.
What are the main complications of a spinal fusion?
The main complications of a spinal fusion are damages that can occur during the placement of the spinal fusion materials. These damages can affect nerve elements or neighboring organs. The kind of the complication depends on the part of the spine that is stabilized with the spinal fusion.
Therefore, in the cervical spine, a damage can occur in a cervical nerve root, the cervical bone marrow (extremely rare complication), the recurrent laryngeal nerve (hoarse voice), cervical sympathetic chain (Horner’s syndrome), or the injury of the esophagus, the trachea, the carotid artery, or the jugular veins.
In the thoracic spine, damage can occur in a thoracic nerve root (intercostal neuralgia), the thoracic bone marrow, or the rupture of the thoracic aorta, pneumothorax (due to an injury in the lung), and so on.
Finally, in the lumbar spine, an injury can occur in a lumbar nerve root. Moreover, there can be non-neurological complications, such as the damage of the dura mater and the leak of cerebrospinal fluid.
Furthermore, besides the neurological complications, a spinal fusion can have more complications, such as bleeding, the creation of a postoperative hematoma, contamination of the surgical wound, the creation of a pseudojoint, and the movement of the spinal fusion materials, among others.
The number and severity of possible complications following a spinal fusion is regularly decreased thanks to the use of modern assistant techniques, such as neuronavigation and the neuromonitoring .






