Bone marrow and spinal cord tumors
Bone marrow and spinal cord tumors are relatively rare. Primary tumors originate from the bone marrow (BM), vertebrae, or the intervertebral discs. Secondary tumors, these are cancer metastases, originate from other body parts. Tumor development differs and may be very fast, as in malignant tumors or extremely slow, as in benign tumors that can develop over the course of several years before the manifestation of any symptom.
Symptoms
Pain is the most common symptom of a tumor and it hurts even more at night or at waking up. It may also reflect to the legs or arms, and it usually gets worse as time passes by and painkillers don’t work. Other symptoms include partial (paresis) or complete (paralysis) limb muscle weakness, posture and walking disorders with possible falls, difficulty in small movements, decreased perception of pain and hot and cold, bladder and bowel incontinence, and spine deformity.
Classification
BM tumors are classified according to their position in the spine, as follows:
Extradural tumors (75%)
The most common extradural tumors are prostate, lung, and kidney cancer metastases. Back pain may be the first symptom of this disease in patients with spine metastatic cancer.
Primary extradural tumors originating from the spinal column bones are more rare. From those, osteosarcoma is the most common type of bone cancer in children while Ewing sarcoma is a particularly aggressive tumor that is developed in young adults. Multiple myeloma is a type of cancer originating from the bone marrow and is more frequently developed in the elderly. Benign tumors, such as the osteoma, the osteoblastoma, and the hemangioma that can cause chronic pain, and scoliosis or neurological symptoms can also be developed in the spinal column bones.
Intradural-extramedullary tumors (20%)
These tumors originate either from the BM arachnoid meninx cells, called meningiomas, from the spinal nerve roots coverings, called neurinomas, or from the ependymal cells in the fourth ventricle, called ependymomas. Meningiomas are more prevalent in females over 40 years old and are usually benign but they locally relapse, especially if they are not completely removed. Neurinomas are also benign but they can transform to malignant as time passes by. Ependymomas are often very big and their complete removal may be deemed impossible due to the cauda equina involvement.
Intramedullary tumors (5%)
These tumors originate from the glial (supportive) cells and are usually astrocytomas (in children) or ependymomas (in adults). Intramedullary tumors can be either benign or malignant and intramedullary metastases are extremely rare. During differential diagnosis of intramedullary tumors, demyelinating disease (Multiple Sclerosis) and transverse myelitis are included. These cases are conservatively treated, without a surgical treatment, and they usually have better rates in comparison with intramedullary tumors. Sternal puncture for cerebrospinal fluid sampling and testing is required for the diagnosis while large dosage of cortisone is administrated for the treatment.
Causes
The cause of bone marrow and spinal cord tumors development is not entirely known. Mutation of various genes has been found in these tumors but the reason behind this mutation is yet to be found. These tumors can rarely be developed in multiple family members in a syndrome context, such as the Neurofibromatosis type 2 (combination of vestibular schwannoma and meningiomas or intramedullary tumors) and Von Hippel-Lindau disease (combination of central nervous system hemangioblastomas with kidney or adrenal gland tumors).
Diagnosis
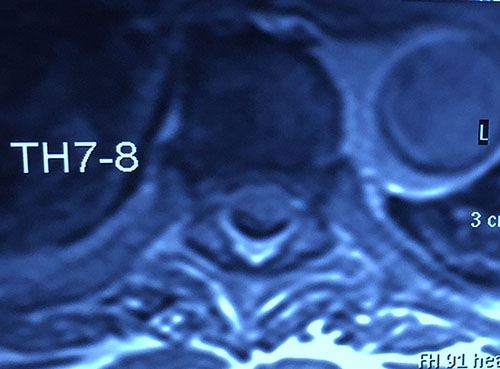
MRI image of an 82-year old patient with an intradural-extramedullary tumor (meningioma Grade I according to WHO)
[image taken from my personal archive]

MRI image of an 82-year old patient with an intradural-extramedullary tumor (meningioma Grade I according to WHO)
[image taken from my personal archive]
Bone marrow and spinal cord tumors are rare and their symptoms are similar to those of other issues (injuries, herniated discs, etc.), thus their diagnosis can be extremely hard. Due to this reason, the detailed medical history of the patient and a detailed neurological exam are required by the neurosurgeon as well as diagnostic tests that will confirm the diagnosis and will locate the tumor. Magnetic Resonance Imaging (MRI) is the optimal test because of the high-resolution imaging of all the anatomic structures of the spine and the bone marrow. A computed tomography (CT) scan is required for the definition of the vertebral infiltration degree as well as the preoperative planning.
In case the patient may suffer from a demyelinating disease or transverse myelitis, sternal puncture for cerebrospinal fluid testing is required while a bone scintigraphy is required for the definition of the metastatic tumors. Finally, a CT-Guided Biopsy is required for the histological identification of the spinal cord tumors.
Treatment
The optimal treatment of a bone marrow or a spinal cord tumor is its complete removal and the possible spinal stability recovery (spinal fusion) along with the simultaneous protection of the BM nerve roots. The following parameters are taken into account for the choice of the most suitable treatment method: the patient’s general health condition, their neurological symptoms, their age, the cancer type and its position, as well as whether it is a primary or a metastatic tumor.
Treatment options include:
A) Health monitoring
These tumors are usually discovered by chance during irrelevant medical exams and long before they cause any symptom. Moreover, small benign tumors that do not compress the BM or the spinal nerve roots significantly but only cause partial symptoms hold a high intraoperative risk and are only treated with health monitoring.
The same treatment is also chosen for old patients as well as for those who may suffer permanent neurological damage caused by surgical treatment or radiotherapy.
An MRI scan is repeated regularly (usually every six months or in case of worsening symptoms) in order to monitor the patient’s health condition.
B) Surgical treatment

MRI image after surgical removal of the meningioma in the bone marrow that is depicted in the previous images
[image taken from my personal archive]

MRI image after surgical removal of the meningioma in the bone marrow that is depicted in the previous images
[image taken from my personal archive]
This method is chosen when the benefit after the removal of a BM or spinal cord tumor is bigger than the risk associated with the postoperative neurological exacerbation. Nowadays, the modern technique of intraoperative neuromonitoring, the use of ultrasonic tools (CUSA), the surgical microscope, the endoscope, and the microsurgery instruments allow us to completely remove tumors that could not be surgically removed before. However, even with the use of all of this equipment and the modern techniques, complete removal of tumors is not always possible. Surgical removal seems to be the best choice for most of the intradural-extramedullary tumors, but tumors such as ependymomas may be impossible to completely remove from the BM or the cauda equina nerves.
Most of the benign tumors are usually removed completely but this isn’t always the case with metastatic or invasive intramedullary tumors. The indicated treatment for metastatic tumors is radiotherapy. Surgery is recommended only in the case of progressive neurological deterioration or instability of the spine. Rehabilitation after surgery can take weeks or months, during which, symptoms are often worse compared with those of the preoperative state.
C) Radiotherapy
Radiotherapy can be used postoperatively to control the residual disease or to prevent recurrence, or to deal with inoperable tumors. It is also used as an emergency treatment for metastatic tumors. Moreover, it can also be used to relieve pain when there is no possibility of cure. Side effects of radiation, such as dizziness and nausea, are adequately treated with medication. In radiotherapy of the spine, targeting techniques are applied as well as segmentation of the dose over several sessions is done, in order to prevent damage to surrounding tissue and improve the effectiveness of treatment.
D) Chemotherapy
Chemotherapy has not proven beneficial for most BM and spinal cord tumors. However, in some cases, chemotherapy is recommended but in combination with surgery and/or radiotherapy.






